Featured
- Get link
- X
- Other Apps
Blue Cross Blue Shield Authorization
Keep the letter for future reference. Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association.
 30 Printable Blue Cross Blue Shield International Medical Claim Form Templates Fillable Samples In Pdf Word To Download Pdffiller
30 Printable Blue Cross Blue Shield International Medical Claim Form Templates Fillable Samples In Pdf Word To Download Pdffiller
An authorization review can take between 2 to 3 business days to complete.
Blue cross blue shield authorization. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. These reviews use evidence-based clinical standards of care to help determine whether a benefit may be covered under the members health plan. If you wish to authorize a person or entity to receive your PHI please complete the information below.
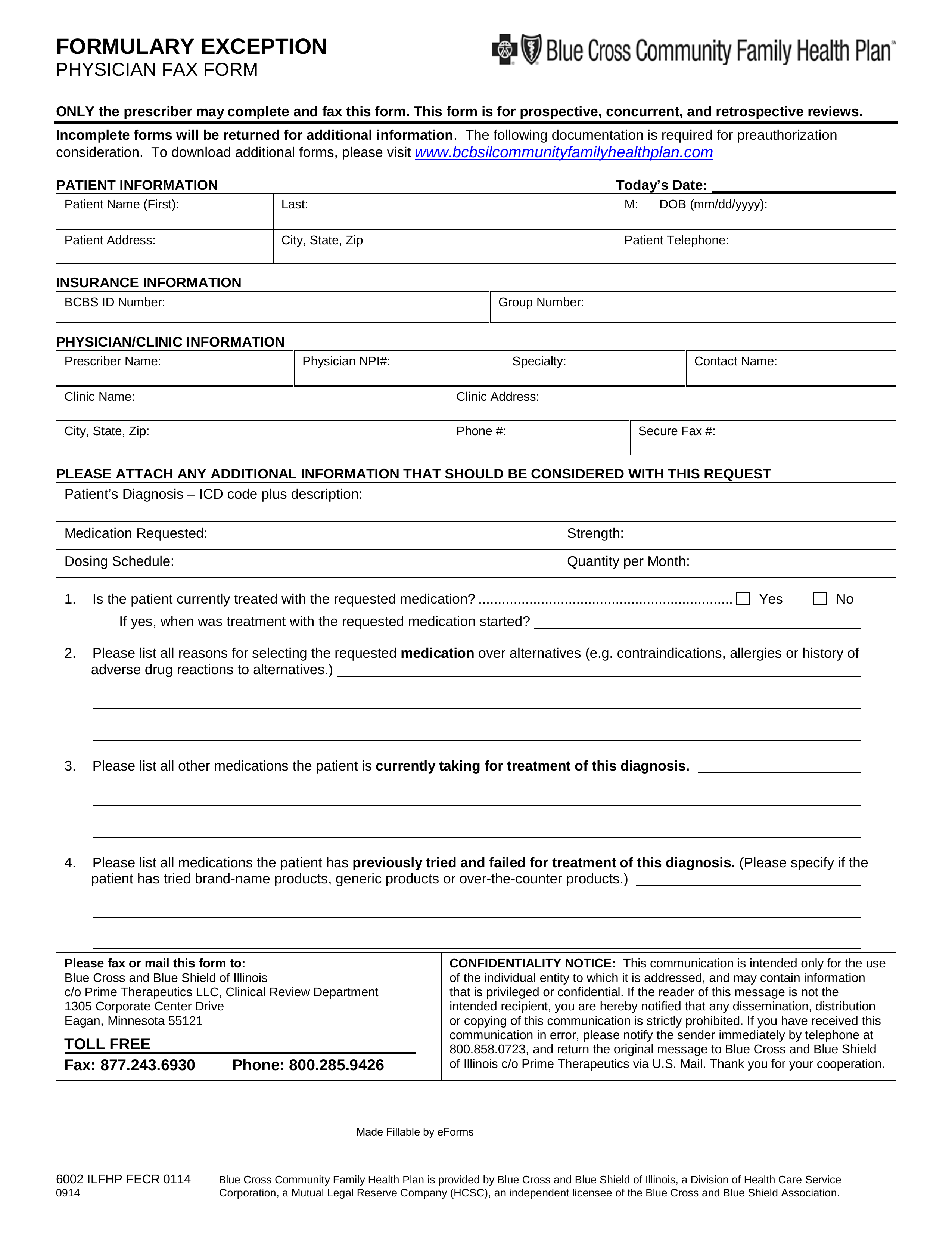
Medicaid only BCCHP and MMAI Predetermination Request Form. Youll Receive a Notice. This page provides Blue Cross Blue Shield of Michigans authorization requirements including information that applies to.
Members Authorization Request Form Commercial Operations IDC You may give Blue Cross and Blue Shield of North Carolina BCBSNC written authorization to disclose your protected health information PHI to anyone that you designate and for any purpose. Medicare Plus Blue SM PPO. Forms are updated frequently.
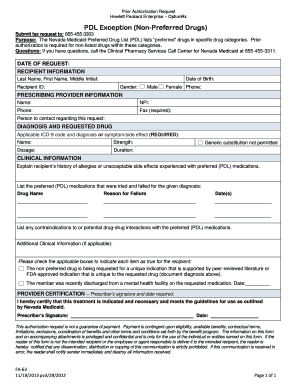
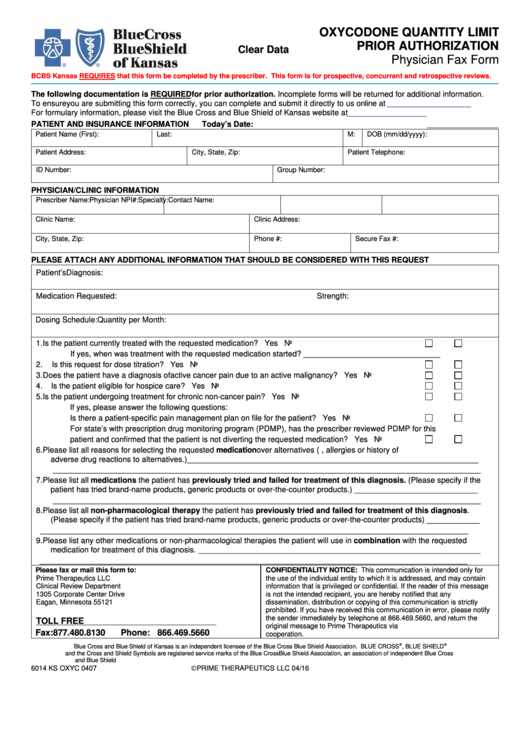
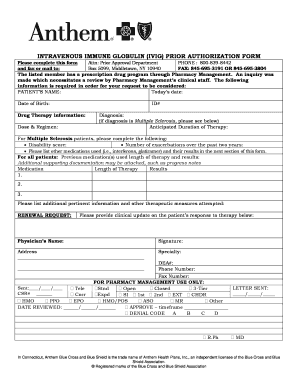
Pharmacy Prior Authorization Request Form Do not copy for future use. Anthem Blue Cross Blue Shield Prior Rx Authorization Form The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a. Utilization management also may include post-service review.
Always check benefits through the Voice Response Unit VRU or My Insurance Manager SM to determine if prior authorization is required. Types of utilization management review that may be conducted before services are rendered include prior authorization predetermination and pre-notification. When prior authorization is required you can contact us to make this request.
Find authorization and referral forms. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Prior authorization sometimes called pre-certification is how Blue Cross and Blue Shield of Minnesota makes sure the treatment your doctor prescribes is medically necessary and helps ensure you are getting proper care.
Florida Blue will mail you a letter confirming that your medical service have been approved or denied. Office notes labs and medical testing relevant to the request that show medical justification are required. Medicaid Prior Authorization Request Form.
Many of our plans require prior authorization for certain procedures and durable medical equipment. For Blue Cross PPO commercial members. You may give Blue Cross and Blue Shield of North Carolina Blue Cross NC written authorization to disclose your protected health information PHI to anyone that you designate and for any purpose.
Blue Cross Blue Shield of Arizona Mail Stop A115 PO. For some services listed in our medical policies we require prior authorization. To determine if a pharmacy authorization is required for a commercial member navigate to the drug formularies page on Blue Shields member website and locate the members plan type.
Blue Cross commercial PPO only. Blue Cross and Blue Shield of New Mexico BCBSNM has contracted with AIM to provide certain utilization management preauthorization services for certain Commercial Retail and ASO members and Blue Cross Community Centennial Members. We use established clinical guidelines to confirm medical necessity when your health plan requires prior authorization.
If you wish to authorize. Physicians must complete and submit a request form for all PA and ST medications. Non-Formulary Exception and Quantity Limit Exception PDF 129 KB Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB.
To verify coverage or benefits or determine pre-certification or pre-authorization requirements for a particular member call 1-18006762583 or send an electronic inquiry through your established connection with your local Blue Plan. Prime Therapeutics our pharmacy benefit manager conducts all reviews of PA and ST requests from physicians for Blue Cross and Blue Shield of Oklahoma BCBSOK members with prescription drug coverage. Benefits will apply if the member meets specified criteria.
Information on requesting authorization Blue Cross. Providers can also view Blue Shields online prior authorization list or telephone Blue Shield. If the request has not been approved the letter will tell you the steps to appeal the decision.
Outpatient Prior Authorization CPT Code List 072 Prior Authorization. Box 13466 Phoenix AZ 85002-3466 Page 1 of 2 Member Information. Prior authorization is required for the medications listed in these policies when administered in a clinicians office or outpatient setting and billed under the members medical benefits.
For a Medicare member navigate to the Formulary drugs in the plan page on Blue Shields member. This process allows us to check ahead of time whether services meet criteria for coverage by a members health plan.
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Https Providers Bcbsal Org Portal Documents 10226 301829 General Prescription Drug Coverage Authorization Request Form A9b9b8bf 922b 469a B21f E396da68c634 Version 1 5
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
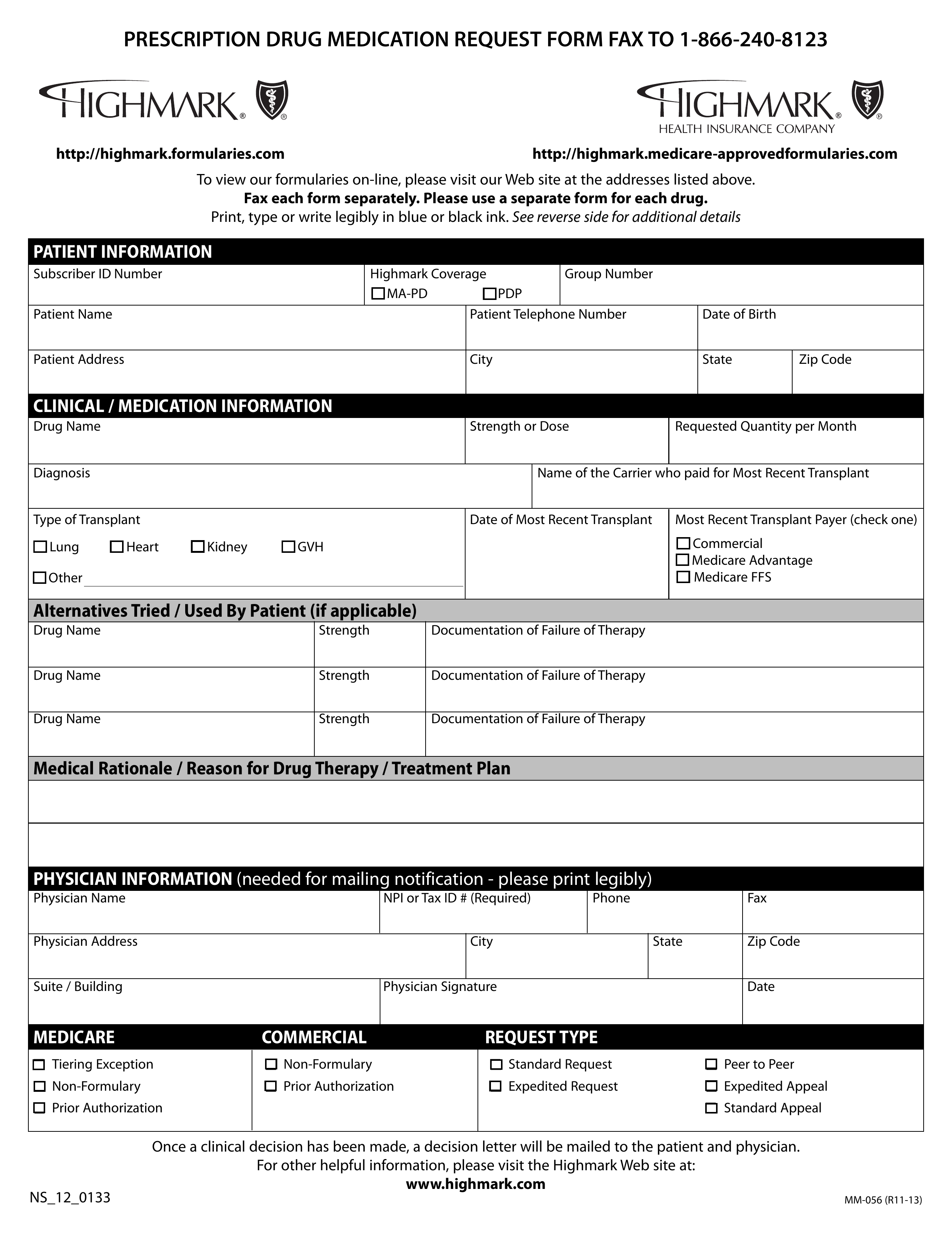 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
Https Www Blueshieldca Com Bsca Bsc Public Common Portalcomponents Provider Streamdocumentservlet Filename Prv Fep Medical Injectable Drug Pdf
Https Bluecrossnc Com Sites Default Files Document Attachment Common Pdfs Hmo Ppo General Quantity Limitations Fax Request Form Pdf
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
Comments
Post a Comment